Overview
Post-streptococcal glomerulonephritis (PSGN) is a rare kidney disorder that develops after bacterial infection with group A streptococci. It results from the body’s immune response against infections such as strep throat, scarlet fever, and impetigo.
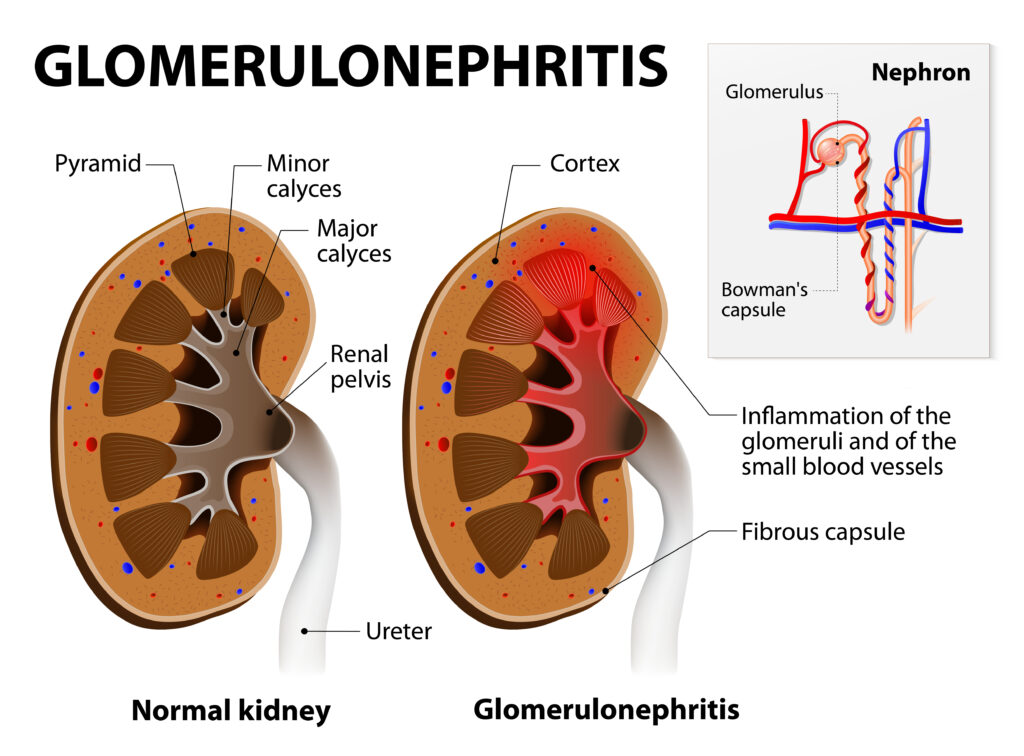
The entry of group A streptococci into the body triggers the immune system to release antibodies that bind with the streptococcal antigens to form immune complexes deposited in the kidney glomerulus, a group of interwoven capillaries within the nephrons of the kidney that filters blood and make urine. These complexes cause the tiny blood vessels in the kidney glomerulus to become inflamed. Consequently, the kidney cannot filter blood passing through the glomerulus, affecting urine production.
PSGN occurs due to an immune response, so a person cannot contract it. However, the bacteria (group A streptococci) can be transmitted to others through infectious respiratory droplets.
Key Facts
- Post-streptococcal glomerulonephritis results from a bacterial infection that causes a loss of kidney function. It is due to an inflammatory response following streptococcal infection.
- PSGN is common in children, and symptoms occur one to two weeks after a streptococcal throat infection or three to four weeks after a streptococcal skin infection.
- Strep throat and impetigo predispose an individual to this condition. Group A streptococci initially affect the skin or oropharynx to cause impetigo( a contagious skin disease) and pharyngitis( sore throat), respectively.
- 50% of children with PSGN show no symptoms and are diagnosed during a routine urine analysis.
- Hematuria (dark, reddish-brown urine), hypertension, and oedema are usually the predominant symptoms.
- Poor hygiene, overcrowding, and low socioeconomic status are risk factors for streptococcal outbreaks.
- Generalized oedema due to fluid retention and anuria, which suggests the failure of the kidneys to produce urine, are life-threatening symptoms that occur in severe cases of PSGN.
- It is suspected in children with hypertension and heart failure, even without hematuria or sore throat.
- Treatment focuses on managing symptoms. PSGN often goes away after several weeks. But, in some adults, symptoms may worsen, leading to end-stage kidney disease and chronic liver failure.
Symptoms and Diagnosis
Symptoms
Some people show no symptoms of PSGN, especially children.
Symptoms, when present, may include:
- Rashes
- Joint pain
- Fatigue (tiredness)
- Nausea or vomiting
- Loss of appetite (anorexia)
- General body discomfort (malaise)
Most patients show signs of a nephritic syndrome, such as:
- Blood in the urine (hematuria) is seen weeks after infection.
- Decreased urine output (oliguria). Less than half of patients experience this symptom.
- Hypertension: Sixty to eighty per cent of patients experience high blood pressure, which goes away within ten days.
- Anuria, the absence of urine, is suggestive of renal failure and occurs in severe cases of this disorder.
- Periorbital oedema (swelling in the eyelids) that is prominent in the morning and disappears at the end of the day.
- Swelling in the legs (oedema) due to fluid retention.
- Respiratory distress syndrome occurs because of pulmonary oedema.
Possible complications as a result of PSGN include:
- Acute renal failure: The inability of the kidneys to remove waste and balance the fluid and electrolyte composition of the body.
- Chronic glomerulonephritis (long-term inflammation of the glomeruli).
- Hyperkalemia: Abnormally high potassium level in the blood.
- Deep vein thrombosis or pulmonary embolism due to blood clots.
- Heart failure
- End-stage renal disease.
Diagnosis
Half of the children with PSGN are asymptomatic and diagnosed during a routine urine analysis. However, some patients may never exhibit any respiratory tract infection symptoms. Meanwhile, recent streptococcal infections, such as sore throat and impetigo, are commonly observed.
Additionally, a physical examination may reveal oedema, which sometimes may be generalized.
Laboratory investigations are helpful in the diagnosis of post-streptococcal glomerulonephritis.
These tests include:
Blood tests: These procedures reveal evidence of streptococcal infection. Renal function tests show blood urea nitrogen (BUN) and serum creatinine levels are usually elevated during the acute phase of PSGN. Similarly, blood tests can detect antibodies like anti-DNAse and anti-hyaluronidase, which are always elevated after the inflammation of the pharynx (pharyngitis) and skin infection.
Urine analysis: This test checks for blood or protein in the urine. White blood cell casts and cellular casts are commonly present in the urine of patients with PSGN and are discovered with the help of urine analysis.
Imaging studies: The imaging tests used to diagnose PSGN include:
- Ultrasonography: It shows the size of the kidneys and any obstruction.
- Chest X-ray: This procedure may show pulmonary congestion in patients with heart failure.
Causes and Prevention
Causes
Post-streptococcal glomerulonephritis is caused by the body’s reaction to infection by bacteria (group A streptococci). This infection occurs in body parts other than the kidneys, such as the skin or throat. An infection in these body parts affects the kidney glomerulus, which filters blood and produces urine. As a result, the kidneys become incapable of carrying out their function of producing urine.
PSGN can affect individuals of all ages but is most common in children between six and ten.
Risk factors of this disorder include:
- Infections include strep throat, impetigo (a contagious skin infection), HIV, and endocarditis.
- Immune system issues, e.g., lupus
- Defective blood vessels
- Family history of kidney disease
- Past or current kidney problems
- Other health-related problems, such as diabetes and hypertension
- Certain medications and exposure to toxins
- Poor hygiene
- Overcrowding
Prevention
The best way to prevent post-streptococcal glomerulonephritis is by preventing group A streptococcal infections like strep throat, scarlet fever, and impetigo.
Some preventive measures include:
Good hygiene
You can reduce your risk of PSGN by embracing proper hygiene, such as:
- Proper hand washing with soap and water for at least 20 seconds.
- Adequate covering the mouth and nose with a tissue when sneezing and coughing and discarding used tissue immediately.
- Using alcohol-based hand sanitiser.
- Washing drinking glasses and utensils properly after every use. Avoid sharing these items with someone who is sick.
Early treatment of streptococcal infections with antibiotics
This measure also helps prevent post-streptococcal glomerulonephritis. Treatment must be according to the prescription and dosing of the doctor.
Typical Treatments
There is no specific treatment for PSGN. Treatment focuses on managing symptoms and depends on the condition’s severity. While mild cases can resolve with little or no treatment, severe cases require treatment targeting symptoms and complications.
Some treatment methods for PSGN include:
Antibiotics: Patients with diagnosed infections by group A streptococci are given antibiotics like penicillin.
Diuretics: Loop diuretics (furosemide) help treat fluid retention (oedema) and hypertension.
Antihypertensive medications: A calcium channel blocker is recommended for uncontrolled blood pressure, which PSGN can cause. Doctors may recommend angiotensin receptor blockers(ARBs) for patients with normal glomerular filtration rate(GFR) and near-normal blood potassium levels.
Dialysis: Fluid and electrolyte balance is maintained as waste products are removed from the blood. This method is recommended in severe cases where kidney failure sets in.
Conclusion
Post-streptococcal glomerulonephritis (PSGN) is due to the immune system’s response to streptococcal infection. The kidney glomerulus becomes inflamed, leading to a reduction in kidney functions.
This condition is common in children, and symptoms occur a few weeks after a streptococcal throat or skin infection.
Treatment depends on the cause and the severity of the symptoms.
MOST COMMON
