Overview
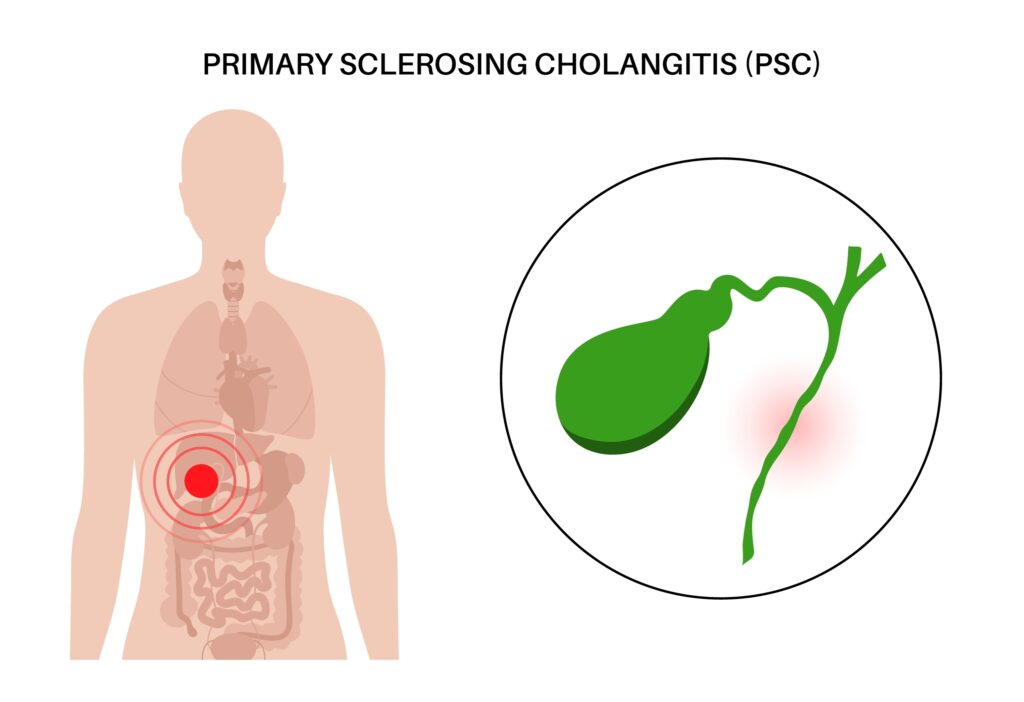
Primary sclerosing cholangitis (PSC), also known as sclerosing cholangitis, is a rare disease of the bile ducts and gallbladder. It is characterized by inflammation and scarring of the bile ducts within (intrahepatic) and outside the liver (extrahepatic). The scar formed in these ducts narrows their width, restricting bile flow.
Obstruction in the release of bile into the gallbladder for storage and the small intestine for the breakdown of fat causes the accumulation of bile in the liver. This occurrence leads to the gradual destruction of the liver cells. Consequently, liver failure may occur.
There is also an increased chance of bile duct infection (acute cholangitis) due to poor drainage of the bile ducts.
Key Facts
- PSC is a progressive condition highly associated with inflammatory bowel disease (IBD), such as ulcerative colitis. 75% of individuals diagnosed with sclerosing cholangitis have IBD.
- It is a rare condition as it occurs in 1 out of every 10,000 people per year worldwide.
- Most people show no symptoms or signs of the condition until a liver function test reveals liver abnormality. The signs and symptoms are always unclear and non-specific and change as the disease progresses.
- The main cause of the disease is unknown, but genetics and environmental factors are known to play a role.
- A family history of primary sclerosing cholangitis increases one’s risk of developing the disease.
- People with PSC have a greater chance of developing bile duct cancer (cholangiocarcinoma).
- This progressive bile duct-related liver disease has no cure. Treatment is aimed at managing complications and preventing further damage. Life expectancy after diagnosis is between 10-20 years.
- A liver transplant is suggested when the liver can no longer perform its functions. However, PSC may return even after a liver transplant causing the transplanted liver to fail.
Symptoms and Diagnosis
Symptoms
Many people diagnosed with primary sclerosing cholangitis may never show symptoms at the time of diagnosis and may continue without symptoms for many years. Symptoms may develop slowly, becoming more severe as the condition progresses.
Initial symptoms of PSC may include:
- Extreme tiredness (fatigue)
- Abdominal discomfort
- Itchy skin (pruritus)
Late symptoms of PSC may include:
- Swollen abdomen
- Enlarged spleen (splenomegaly)
- Enlarged liver
- Fever
- Jaundice: Yellowing of the sclera (white of the eyes) and skin
- Weight loss
Complications due to excessive scarring and failure of bile ducts include:
- Metabolic diseases: The condition may manifest as metabolic conditions, such as fatty stools, diarrhea, malnutrition, thinning bones, and poor night vision. Since bile is important for the breakdown of fat and absorption of fat-soluble vitamins (A, D, E, and K), the digestion and absorption of fat cannot be complete without it.
- Portal hypertension: The liver cells are destroyed due to the backflow of bile. This causes damage to the liver tissues and obstruction of portal blood flow. The pressure in the portal vein is raised, leading to increased pressure in other veins. This high blood pressure may cause fluid to leak into the abdominal cavity (ascites) or bleeding from blood vessels.
- Bile duct cancer (cholangiocarcinoma): Advanced PSC raises the risk of developing cancer of the bile ducts.
- Liver failure: Prolonged inflammation of the bile ducts present in the liver results in the destruction and scarring of the liver tissue and a loss of liver functions.
Diagnosis
Primary sclerosing cholangitis (PSC) is often suspected during a routine blood test that shows an abnormal rise in the enzymes produced by the liver cells, an indication of liver damage. To confirm PSC, healthcare providers may propose a specific test: a blood test or imaging test.
Specific tests for PSC include:
- Liver function test: This blood test checks for certain enzymes produced by the liver: alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase. An elevated amount of these enzymes indicates PSC.
- Magnetic resonance cholangiopancreatography (MRCP): This non-invasive test uses magnetic resonance imaging techniques to make images of the liver, bile ducts, and gallbladder. It is accurate and the first test used to diagnose primary sclerosing cholangitis.
- Endoscopic retrograde cholangiopancreatography (ERCP): An endoscope is used to inject dye into the bile, and X-ray pictures that reveal the narrowing of the bile ducts are taken.
- Liver biopsy: This test is also used for PCS diagnosis. It indicates the extent of damage to the liver and is used when the diagnosis is still uncertain. A small sample of the liver tissue is removed and sent to the laboratory for testing.
Causes and Prevention
Causes
The primary cause of this disease is unknown, but a combination of genetic and environmental factors may play a role. There is evidence that a change in genes involved in immunity, such as human leukocyte antigen (HLA), is associated with the condition.
Risk factors may include:
- Sex: PSC affects men twice as often as women.
- Age: It is found in all ages but is commonly diagnosed in young individuals between 30 and 40.
- Inflammatory bowel disease (IBD): 75% of individuals with sclerosing cholangitis also have ulcerative colitis.
- Family history of the disease: Family members of someone diagnosed with PSC have a higher risk of developing the condition.
Prevention
There are no preventive measures for primary sclerosing cholangitis due to its unknown cause. However, the progression of the disease into cholangiocarcinoma (bile duct cancer) can be prevented through a liver transplant.
Typical Treatments
Primary sclerosing cholangitis cannot be cured. Treatment is aimed at managing symptoms and complications, and opening blocked bile ducts to prevent further destruction of the liver. Still, the damage already present cannot be reversed.
The usual management procedures for PSC include:
- Treatment for itching: Bile acid sequestrants are used to treat PSC-associated itching. These medications bind to bile acid, responsible for the itching in liver disease.
- Treatment for metabolic diseases: Vitamin supplements are recommended for treating certain metabolic diseases linked to PSC.
- Treatment for narrowed bile ducts: Balloon dilation with a balloon catheter is used to open extrahepatic ducts (ducts outside the liver).
- Liver transplant: A liver transplant may be performed if the liver completely loses its functions.
Conclusion
Primary sclerosing cholangitis occurs due to an inflammation of the bile ducts. It is a rare disease with an unknown cause, but more likely to occur in people with a family history of the disease.
There is no cure for the disease, and liver failure may eventually occur.
MOST COMMON