Overview
Cervical cancer is a health condition that develops in a woman’s cervix (the entrance to the womb from the vagina). This cancer usually affects sexually active women of 30 -45 years.
Cervical cancer is majorly caused by different strains of the human papillomavirus (HPV), a sexually transmitted infection.
When infected, the body’s immune system typically tries to fight off the virus. However, in some cases, some strains survive and live in the body for years, turning the cervix cells cancerous.
You can reduce the risk of developing this health condition by getting vaccinated against HPV.
Key facts
- The cervix is the narrow part of the uterus (womb) in a woman’s body that opens into the vagina.
- A sexually transmitted disease called HPV is responsible for nearly all cases of cervical cancer.
- Cervical cancer can be prevented with the HPV vaccine.
- An HPV infection can cause the cervix cells to change and grow, a condition known as cervical dysplasia, which is precancerous.
- Cervical cancer is the only one out of the gynaecological cancers with a Pap test (Pap smear) screening test.
- Cervical cancer is very treatable when diagnosed early.
Symptoms
Cervical cancer usually does not present any symptoms until it has reached an advanced stage. This is why you must attend all your cervical screening appointments.
More often than not, abnormal vaginal bleeding is the first noticeable symptom of cervical cancer.
These include:
- Bleeding during or after sex, between periods, or after menopause
- Difficult or painful and sometimes bloody urine.
- Diarrhoea, or pain or bleeding from your rectum when pooping.
- Fatigue, loss of weight, and appetite.
- A general feeling of illness.
- Dull backache or swelling in your legs
See your doctor for advice if you experience any type of abnormal vaginal bleeding.
Diagnosis
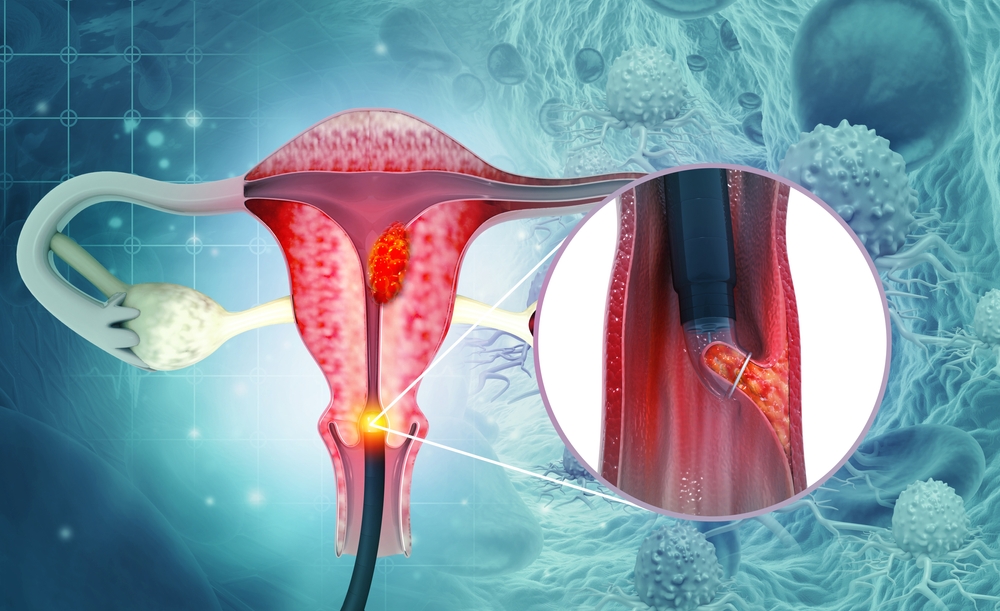
When cervical abnormalities are found through regular pap smear tests or the symptoms present themselves, there are several biopsy options to diagnose cervical cancer. Some biopsies can remove abnormal tissue growth from the cervix, making them treatment options for precancerous lesions.
For some biopsy procedures, you will be required to go under local anaesthesia, while others require general anaesthesia. Several types of cervical biopsies include:
The different types of cervical biopsies include:
- Loop electrosurgical excision procedure (LEEP): An electric wire is used to loop and obtain a piece of tissue from the cervix for examination in a lab.
- Colposcopy: A procedure that uses an instrument called a colposcope. A colposcope is fitted with magnifying lenses used to examine the cervix for abnormalities. If any irregularities are found, a biopsy is conducted utilising colposcopy.
- Endocervical curettage: This procedure uses a narrow instrument called a curette to scrape the lining of the endocervical canal. It is usually performed and completed with a colposcopic biopsy.
- Cold knife cone biopsy: The cone knife biopsy procedure uses either a laser or surgical scalpel to extract a piece of cervical tissue for further examination under a microscope. You will need to go under general anaesthesia for this procedure.
- Cone biopsy (also called conization): This biopsy diagnosis process uses the cold knife or the loop electrosurgical excision or removes a larger, cone-shaped piece of tissue from the cervix. The cone biopsy procedure is also a treatment option for precancerous lesions and early cancers.
- HPV DNA test: This test is done to detect cervical HPV infection. The cervix cells are collected for a regular Pap test, but it is not a replacement for a Pap test. The HPV DNA test may be used as a screening test for women over 30 or women with slightly irregular Pap test results to determine if further testing or treatment is required.
Causes
HPV is the cause of nearly all cases of cervical cancer. HPV is a prevalent virus that can be passed on through any sort of sexual contact with a man or a woman.
There are over 100 strains of HPV, and many of them are harmless. However, some HPV strains can cause abnormal changes to cervix cells, eventually leading to cervical cancer.
These two strains known to be responsible for most cases of cervical cancer are HPV16 and HPV18.
They often do not have any symptoms, making it almost impossible for women to detect that they have them. However, these infections are common, and most women who have them do not develop cervical cancer.
Prevention
To reduce your risk of cervical cancer;
- Get the HPV vaccine. Getting vaccinated for HPV to prevent getting the virus will reduce your chances of getting cervical cancer. Ask your doctor or other healthcare providers about the process of getting the vaccine.
- Have routine Pap tests: Pap tests can detect precancerous conditions in the cervix so they can be treated to prevent cervical cancer. Women 21 and above should have a yearly pap test.
- Practice safe sex: To reduce your chances of getting any HPV strains, practice safe sex using condoms. Avoid sex with multiple sexual partners as well.
- Do not smoke: Talk to your doctor about ways to quit if you smoke. if you do not smoke, don’t start
Treatment
Treatment for cervical cancer usually depends on how widespread and advanced the cancer is.
As cancer treatments are often complex, hospitals use multidisciplinary teams (MDTs) to properly diagnose and tailor treatment according to the patient and cervical cancer stage.
MDTs are a team of several specialists who work together to decide the best way to proceed with your treatment.
Your MDTs team will diagnose and recommend the best treatment options, but the decision to choose will be yours.
The options will most likely range from;
- Surgery: For early cervical cancer, a surgery to remove the cervix and some parts or all of the womb, or radiotherapy, or a combination of both will be recommended.
- Radiotherapy: Radiotherapy with or without chemotherapy and surgery is also sometimes used in advanced stages of cervical cancer.
- Chemotherapy: Chemotherapy medications are used to kill cancer cells all over the body. Your doctors will administer this treatment in cycles. Chemo will be administered for some time, after which you will stop using the treatment to allow your body time to recover.
- Targeted therapy: A new drug, Bevacizumab (Avastin), which works differently from chemotherapy and radiation, is used. It blocks the growth and production of new blood vessels that give the cancer juice to grow and survive. Bevacizumab is usually administered alongside chemotherapy medication.
- Palliative care: This treatment is used when cervical cancer is not curable. Certain medications can slow down its progression to prolong lifespan and relieve associated symptoms, such as pain and vaginal bleeding.
If your doctor discovers precancerous cells in your cervix, they can also be treated.
Conclusion
Cervical cancer is a potentially life-threatening cancer that develops in a woman’s cervix. Most cases of cervical cancer are caused by variant strains of the human papillomavirus (HPV). Symptoms include heavy bleeding between and after periods or menopause. Cervical cancer is often curable when discovered at an early stage.
MOST COMMON