Overview
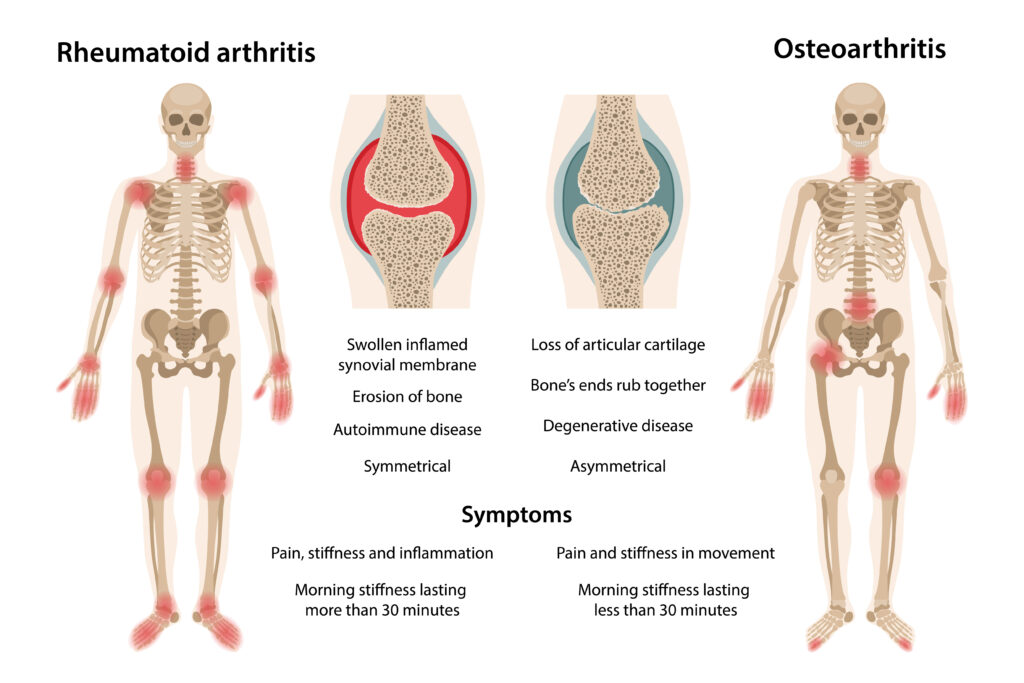
Rheumatoid arthritis (RA) is a chronic autoimmune ailment that causes joint inflammation. It can affect any joint but mainly occurs in the small joints of the wrists, hands, and fingers.
The pain from RA is often worse at night and during cold weather. It may be tender to touch and cause loss of movement in affected joints.
RA occurs when your immune system erroneously attacks cells in your body, especially those that produce proteins called antibodies. A protein known as rheumatoid factor (RF) is typically detected in the blood tests of people with this condition.
According to the World Health Organization, more than 23 million people worldwide have rheumatoid arthritis.
Key Facts
- Rheumatoid arthritis is a chronic, progressive autoimmune condition that affects joints.
- It’s more common in women than men and most commonly affects the large and small joints of the hands, wrists, elbows, knees, ankles, and hips.
- Osteoarthritis (OA) affects up to 95% of people with RA. OA is characterized by joint damage that causes pain and stiffness.
- Rheumatoid factor–positive RA occurs when the body’s immune system attacks its cells, causing inflammation.
- An inflammatory polyarthritis is a distinctive form of RA that affects fewer than 1% of people with RA.
- RA affects more than 23 million people worldwide, according to the World Health Organization (WHO).
- Rheumatic arthritis currently has no cure.
Symptoms and Diagnosis
Symptoms
Rheumatoid arthritis manifests as various symptoms in the subject. There are usually no symptoms for months after the initial period of inflammation begins.
Some of the most common symptoms include:
- Inflammations in the joint
- Stiffness
- Fever
- Sudden loss of weight
- Tiredness
- Joint pains, especially in the morning.
Diagnosis
RA is a progressive, chronic disease affecting the joints. It’s marked by pain and swelling in your hands, wrists, fingers, and feet, called erosions, and can also affect other parts of your body.
Rheumatoid arthritis is difficult to diagnose because it often occurs slowly over months or years.
There’s no specific diagnosis for rheumatoid arthritis.
However, most healthcare practitioners carry out the following diagnostic measures:
- Checking for joint damage to tendons, ligaments, and cartilage.
- Examining stiffness in the joints.
- Anti-citrullinated peptide antibody test (anti-CCP): People who test positive for anti-CCP test likely have RA.
- Checking for pain in the muscles and bones around affected joints.
- Testing muscles for reflexes and damage.
- Performing lab blood tests for Rheumatoid factor.
- Checking for numbness around the fingers.
- Examining the hair for signs of hair fall.
- Carrying out a lab test to check for an altered blood profile.
RA Blood Test
In some instances, a radiographic process must be carried out on some of the patient’s body parts, such as the joints, to examine if there is any sign of rheumatoid arthritis physically.
Aside from radiographic examination, some specific blood tests are carried out on patients suspected of RA.
Some of the most common RA blood tests include:
- Test for C-reactive protein: C-reactive proteins are triggered mainly by inflammations. So, the presence of C-reactive protein may be a sign of RA.
- ESR Test: The erythrocyte sedimentation rate (ESR) test is done to examine the severity of inflammations.
- Antinuclear antibody test: This test checks if the body is still producing antibodies.
- Rheumatoid factor test: The RF test is performed to determine if there is a rheumatoid factor in the blood. Inflammation may be one of the reasons behind the elevated RF in the blood.
Causes and Prevention
Causes
The exact cause of rheumatoid arthritis is unknown. It is thought to be an immune reaction to a trigger in the body.
There are many theories about what causes rheumatoid arthritis, but none have been proven.
Some of the likely causes of RA are:
- Genetics: Some theories suggest a genetic predisposition to autoimmune diseases. Others suggest that infectious agents, such as bacteria or viruses, may trigger an immune response that leads to an autoimmune disease.
- Family history: People with rheumatoid arthritis may have a family member who has already been diagnosed.
- Diet: Your diet eat may expose you to higher risks of rheumatoid arthritis. Foods high in sugar and fructose, red meat, and high iron levels increase the risk of getting the disease.
- Sex: Gender is another factor that exposes people to the risks of contracting the disease. The Centers for Disease Control and Prevention (CDC) suggests that females are twice more likely to contract rheumatoid arthritis than males.
- Smoking: Smoking cigarettes heightens your chances of developing RA. Nursing mothers who smoke also place their unborn children at risk.
- Age: People aged 45 and above are more likely to develop RA.
Prevention
Prevention is the best way to combat rheumatoid arthritis.
There are several things you can do to prevent the disease, including:
Avoid smoking: Avoid smoking tobacco smoke, which is linked to rheumatoid arthritis, other types of inflammation, and cancer.
Avoid excess alcohol intake: Limiting alcohol intake can damage your liver and increase inflammation in the body.
Supplements: Taking vitamin D supplements or other supplements for bone health.
Get a physical examination at least every year: A doctor can check for signs of rheumatoid arthritis, such as swelling in your hands or feet. You should also do blood tests to check for signs of inflammation.
Exercise regularly: Physical activity helps improve your odds of avoiding or delaying the onset of rheumatoid arthritis. It may also curtail your symptoms if you have the disease.
Control your weight: Being overweight increases your risk of developing rheumatoid arthritis. If you’re obese, losing weight could help reduce your chances of getting the disease or slowing its progression over time.
Typical Treatments
Currently, there is no absolute cure for rheumatoid arthritis. However, it can be managed and kept under reasonable control.
Treatment may range from simple rest to surgery, if necessary, combined with medications; however, finding a long-term treatment remains one of the biggest challenges.
A combination of drugs is usually used to manage RA.
Some of these medications include:
- Biologic drugs, such as gold sodium thiomalate, infliximab, or etanercept.
- Non-biologic disease-modifying antirheumatic drugs (DMARDs), such as methotrexate and hydroxychloroquine.
- Oral corticosteroids, such as prednisone or hydrocortisone.
- Oral disease-modifying antirheumatic drugs (DMARDs).
When it comes to the treatment of RA, there is no fundamental approach. Different medical personnel treats the disease based on their expertise and experience.
Conclusion
Almost everyone will develop joint degeneration with age-related wear and tear. Symptoms include swelling, tenderness, stiffness, redness, heat around a joint, and pain during movement or use. In RA, these inflammatory changes occur earlier and faster.
The inflammation usually affects hand joints and those forming part of the wrist (wrist arthritis). With time, deformities may set in.
MOST COMMON