Overview
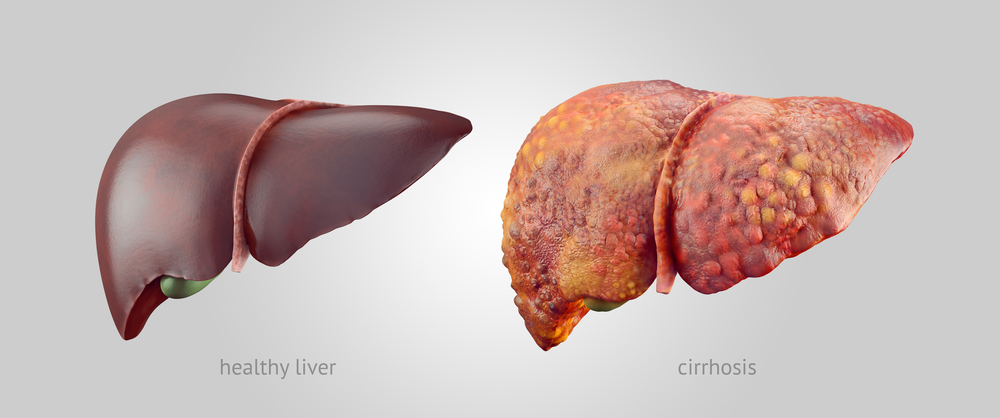
Cirrhosis, hepatic cirrhosis, or end-stage liver disease involves decreased liver function due to the replacement of healthy liver tissue by nonfunctional scar tissue. It is an aftermath of chronic liver disease, a clinical condition caused by the continuous destruction and repair of the liver tissue, leading to impairment of liver functions.
In cirrhosis, the scar tissue obstructs portal circulation increasing blood pressure and normal body function. This occurrence results in severe complications identified with the condition. Though the disease has several causes, chronic hepatitis infection and excessive alcohol consumption are its primary triggers.
Key Facts
- Cirrhosis is irreversible scarring of the liver tissue resulting from an extended period of liver damage.
- The liver may still retain most of its functions even with cirrhosis. However, the patient may eventually experience liver failure.
- Hepatitis B or C infection and excessive alcohol consumption increase an individual’s risk of cirrhosis. About 57% of hepatic cirrhosis cases are attributed to hepatitis, while 20-40% are alcohol misuse.
- Symptoms may never be identified until a serious stage of the condition is reached.
- Based on the appearance of symptoms, cirrhosis can be classified into two clinical stages: compensated and decompensated.
- Early treatment may stop cirrhosis from worsening and curb the gradual harm to hepatic cells.
- A medical practitioner will recommend a liver transplant when the liver has been severely damaged, which happens at the latter end of the decompensated stage.
Stages of Cirrhosis
The replacement of healthy liver parenchyma (functional tissue) by scar tissue is progressive. Similarly, the presence or absence of symptoms depends on the extent of fibrosis and compensation by healthy cells.
The Cleveland Clinic suggests that there are two clinical stages of hepatic cirrhosis.
- Compensated cirrhosis: This stage occurs with little or no symptoms as unaffected cells still perform certain functions and meet the body’s needs, thereby compensating for the destroyed cells. There is a higher survival rate, and life expectancy is around 9-12 years. If the causes are not identified and treated in time, this stage may progress into decompensated cirrhosis.
- Decompensated cirrhosis: It is characterised by the presence of symptoms which are mainly ascites, jaundice, hepatic encephalopathy, and variceal haemorrhage. These symptoms are evident because of the repeated destruction of more liver cells. In this phase, the life expectancy is around 1-2 years. This stage can only be reverted to the compensated stage when the cause of the liver disease is identified and treated promptly. Otherwise, liver failure is inevitable.
Symptoms
The symptoms of end-stage liver disease depend on the specific stage and the extent of the damage.
Early symptoms common in the compensated phase include:
- Loss of appetite
- Weakness
- Stomach discomfort
- Fever
- Weight loss
Serious symptoms are the distinguishing features of the decompensated stage, and they include:
- Variceal haemorrhage: Bleeding of the stomach and oesophagus vessels, known as variceal haemorrhage.
- Hepatic encephalopathy: Loss of brain function due to failure of the liver to get rid of the toxins in the blood.
- Ascites: Accumulation of fluid in the abdominal cavity.
- Jaundice: Yellow discoloration of the eyes and skin.
Diagnosis
To confirm the presence of hepatic cirrhosis, doctors use medical history, physical examination, and a combination of laboratory and imaging tests.
Medical history and physical examination
Your doctor may inquire about your symptoms and use of alcohol and other medication. They may also look for signs of a swollen abdomen, tenderness or pain, yellow skin or eyes, and swollen blood vessels on the skin.
Laboratory tests
The laboratory tests for the diagnosis of cirrhosis include:
- Liver function tests: These procedures reveal the level of liver enzymes, such as alanine transaminase (ALT), aspartate transaminase (AST), and alkaline phosphatase (ALP). In addition, they detect the level of bilirubin and liver proteins in the blood. A rise in these enzymes and bilirubin levels in the blood indicates a liver malfunction. However, a decrease in the blood protein level suggests liver damage.
- Full blood count (FBC): This test can determine the underlying cause of cirrhosis as it diagnoses signs of infection and blood loss. It also shows the severity of the hepatic injury.
Imaging tests
The imaging tests for examining the liver for signs of cirrhosis are:
- Abdominal ultrasound: This test assesses the efficiency of portal blood flow.
- Elastography: A procedure that detects hardening or stiffening of the liver and gives an idea of the severity of fibrosis.
- Magnetic resonance imaging (MRI): MRI shows the structure of the liver and the damage caused by liver diseases, such as hepatitis.
Causes
Some possible causes of cirrhosis are:
- Habitual alcohol misuse.
- Chronic viral hepatitis (hepatitis B and C).
- Fatty liver disease (non-alcoholic steatohepatitis).
- Inherited diseases like hemochromatosis ( iron pileup) and alpha-1 antitrypsin deficiency.
- Inflammation and injury of the bile duct (primary biliary cholangitis).
Prevention
You can reduce your risk of developing end-stage liver disease by following these measures:
- Decrease your alcohol consumption
- Eat a healthy diet consisting of vegetables, first-class proteins, fruits, and whole grains
- Make exercise a constant routine
- Keep a healthy weight
- Shun high-risk behaviors like indiscriminate sex and sharing of sharp objects that expose one to hepatitis B or C infection
- Take medication only on prescription by a registered healthcare provider, and stick to the appropriate dose.
Typical Treatment
The underlying cause is important in the treatment and management of the condition. Although it cannot be cured, proper management of the symptoms can prevent further damage.
To manage the symptoms of cirrhosis, hepatologists may recommend:
- Discontinuing the use of alcohol for alcohol-induced liver disease
- Healthy eating, exercise, and weight loss plans for non-alcoholic fatty liver disease.
- Antibiotics or vaccination as a preventive treatment for hepatitis B or C.
To relieve the complications, treatment options include:
- Transjugular intrahepatic portosystemic shunt (TIPS): This procedure propels blood towards the heart, thereby circumventing blood flow into the liver. It is effective for treating portal hypertension associated with excessive buildup of scar tissues.
- Low sodium diet to control fluid accumulation in ascites. More serious cases of ascites may require fluid drainage.
- Band ligation to control bleeding from swollen esophageal or gastric vessels.
- Liver transplant for severe damage that results in total loss of liver function.
Conclusion
Cirrhosis is a clinical condition characterised by the formation of scar tissues in the liver. Alcohol misuse and hepatitis infections are common causes.
The symptoms depend on the extent of damage to the liver cells. Early diagnosis and prompt adherence to treatment are known to limit the disease progression.
In the case of complete loss of liver functions, a liver transplant becomes the only effective choice.
MOST COMMON