Overview
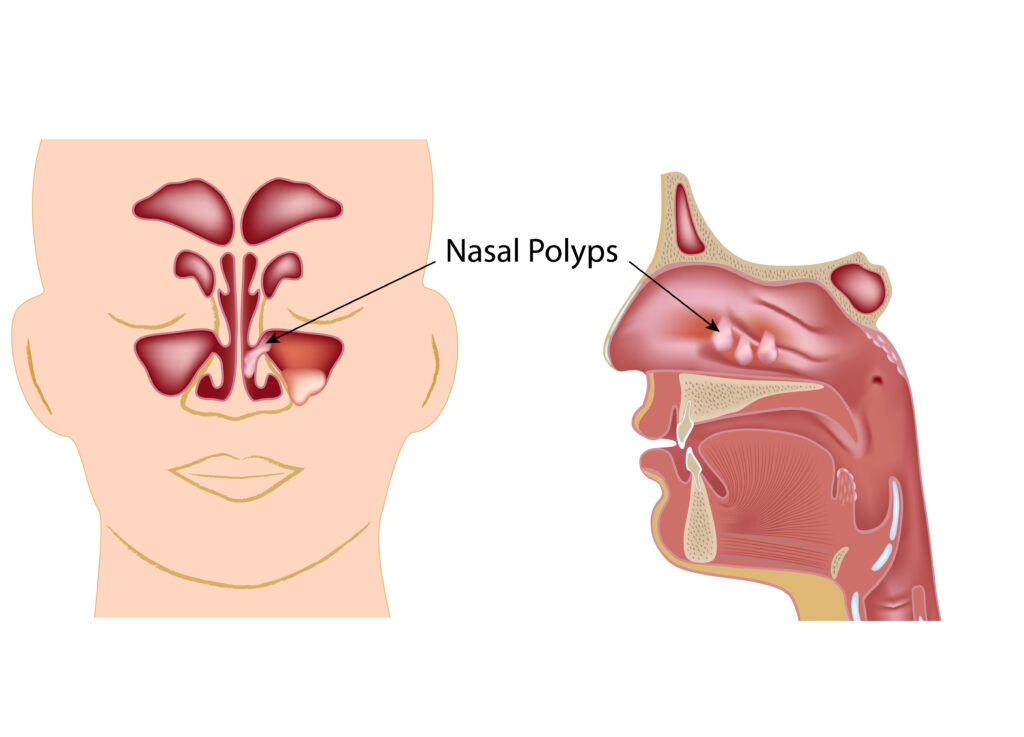
Nasal polyps are soft growths formed from the mucous membranes lining the nasal passages and paranasal sinuses (air-filled spaces connected to the nasal cavity). They are noncancerous and lack nerve sensation (painless).
The nasal mucosa (mucous membrane of the nose) is a well-vascularized wet layer that protects the nose and sinuses and aids respiration. During constant infection or irritation, the mucosa becomes swollen, and fluid accumulates within it, forming benign (noncancerous) growths that may block the nasal cavity passages.
Chronic sinus infection, asthma, allergic rhinitis (hay fever), and drug sensitivity are primary triggers for the development of nasal polyps.
Key Facts
- Nasal polyps are soft, painless, benign growths on the lining of nasal passages or sinuses. They may grow in either or both nostrils at the same time.
- Nasal polyps can affect people of all ages, but they are most common in adults between 30 and 40.
- Continuous irritation and inflammation in the nasal cavity can trigger their formation.
- Asthma, drug sensitivity, and allergies are conditions often associated with these noncancerous growths.
- They affect 4-40% of the general population and are more common in men than women.
- These growths usually occur where the eyes, nose, and cheekbones meet (a point where the upper sinuses drain into the nose).
- Complications of nasal polyps result from the obstruction of airflow and normal fluid drainage. Small polyps may not cause any symptoms. However, as they multiply and increase in size, they may block the nasal passages and sinuses, resulting in chronic congestion and a loss of the sense of smell.
- Medications can reduce inflammation and the size of polyps. For persistent symptoms, surgery is recommended. Still, the polyps may return after surgery.
Symptoms
Small polyps rarely cause any symptoms, but they block the nasal passages and sinuses as they become larger.
The following symptoms are common:
- Frequent nosebleeds
- Runny nose, which may be frequent.
- Nasal stuffiness: The patient may find it difficult to breathe through the nose.
- Poor sense of smell or loss of smell. This may persist even after treatment.
- Snoring
- Poor sense of taste, which may never improve after treatment.
- Postnasal dripping: The feeling of excess mucus running down behind the throat.
- Pressure or pain in the face or upper teeth.
- Headache, which may be due to sinus infection.
- Obstructive sleep apnea: The patient stops breathing during sleep. It occurs in severe cases of nasal polyps.
- Double vision, which also occurs in severe cases.
Diagnosis
Your doctor can diagnose your condition from your answers to specific questions about symptoms (such as allergies, infection, and asthma) and by examining your nose using a lighted instrument. Polyps are often visible with the aid of a lighted instrument.
Other tests to confirm the diagnosis of nasal polyps include:
- Nasal endoscopy: A thin, flexible tube with a camera and light (nasal endoscope) is inserted into the patient’s nose to examine the nasal cavity and sinuses.
- Imaging studies: A detailed picture from computed tomography (CT) and magnetic resonance imaging (MRI) gives the polyps’ size and exact location in the nasal passages and sinuses. This can help rule out other growths, such as cancerous growths which may be more severe.
- Allergy tests: These tests are used to determine the cause of nasal inflammation. Tiny pricks are made in the skin, and different allergens are deposited. Afterwards, the doctor observes the skin for signs of allergic reactions. A blood test can also detect specific antibodies produced against distinct allergens.
- Non-invasive sweat test: This test is performed when young children show signs of nasal polyps. It is a test for a genetic disease called cystic fibrosis, which affects the glands producing sweat, tears, saliva, and digestive enzymes. The child’s sweat is tested, and the components are compared with those present in a healthy person.
Causes
Polyps develop because of a change in the structural integrity of the mucous membranes lining the nasal cavity and sinuses. Allergies and infections, which exist for a long time, produce the inflammation responsible for the change.
Different risk factors are associated with the mucous membranes’ long-term irritation and swelling (inflammation).
They include:
- Asthma, which causes inflammation of the airway.
- Sensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin.
- Cystic fibrosis: A genetic disease that causes an abnormal thickening of the body fluids.
- Vitamin D deficiency
- Allergic rhinitis: Inflammation of the nasal passages and sinuses, which includes hay fever.
- Age: Nasal polyps occur at any age, but young adults are more at risk.
- Genetics: Your family history of nasal polyps affects your chances of developing them.
Prevention
Preventive strategies help decrease your risk and also deter a recurrence after treatment.
These measures include:
- Strict adherence to doctor’s instructions on allergy and asthma medications.
- Avoiding nasal irritants (allergens, tobacco smoke, chemical fumes, and dust), which may irritate the nose and sinuses to cause inflammation.
- Washing hands thoroughly and regularly to prevent bacterial and viral infections.
- Using a saline nasal wash to rinse nasal passages. This helps remove irritants and allergens and enhances the free flow of mucus.
Typical Treatments
According to the Mayo Clinic, the goal of treatment is arresting inflammation and reducing the size of polyps or eliminating polyps completely.
Medications
Medications are normally the first line of treatment for nasal polyps.
They include:
- Nasal corticosteroid: A corticosteroid nasal spray (fluticasone and budesonide) can reduce swelling and decrease the polyps’ size.
- Oral and injectable corticosteroids: Your doctor may prescribe oral corticosteroids such as prednisone when nasal corticosteroids fail to produce the desired effect. Due to side effects, treatment with oral corticosteroids is recommended for a short period. Injectable corticosteroids are used when nasal polyps become severe.
Surgery
Surgery may be employed when medications fail to shrink or eliminate polyps.
The surgical procedure depends on the size of the polyps.
Polypectomy: It is a procedure for removing small nasal polyps. A suction device cuts and removes polyps from the nasal mucosa. Also, small pieces of bones are removed to expand the nasal passageway.
Endoscopic sinus surgery: It is used to remove larger polyps. An endoscope with a tiny camera and cutting tools attached to its end is utilized in this procedure. After surgery, the doctor suggests nasal sprays and anti-allergy medications to help prevent new growths.
Conclusion
Nasal polyps are fleshy growths that develop in the mucosa lining the nose and sinuses. They vary in size and are noncancerous. While smaller polyps may pose no health risk, larger ones can cause breathing difficulty and a poor sense of smell or a total loss of smell.
The purpose of treatment is to stop inflammation, reduce the size of polyps, or completely eliminate them.
MOST COMMON