Overview
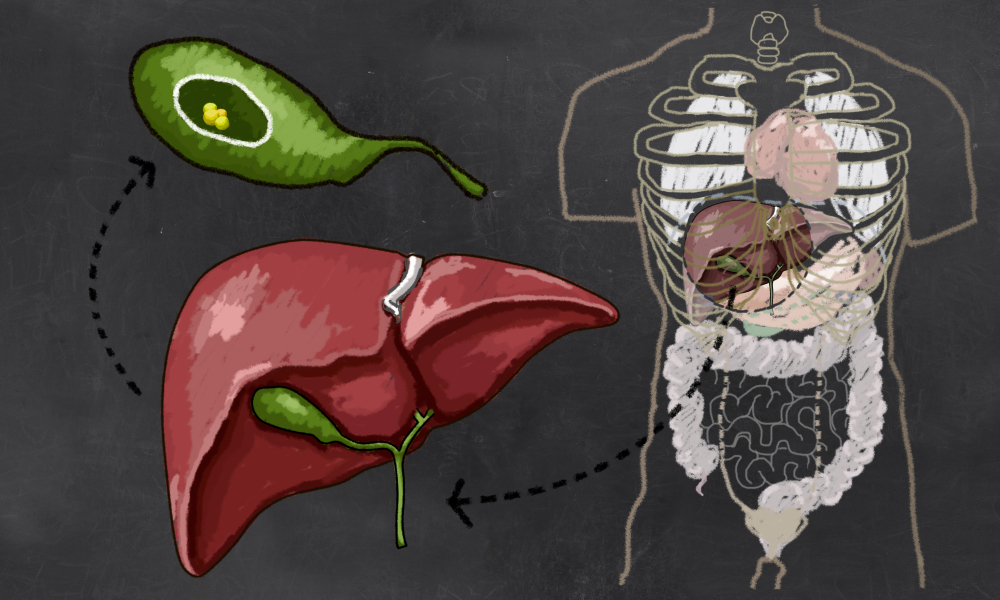
Although the digestive fluid bile is produced in the liver, it can flow backwards into the stomach and, in some cases, into the oesophagus.
Bile reflux may also occur when stomach acid (gastric acid) refluxes into the oesophagus. The latter can lead to gastroesophageal reflux disease (GERD), characterised by chronic oesophageal inflammation and irritation.
It is possible to alleviate symptoms of bile reflux by making some modifications to your diet and way of life, but this is not the case with acid reflux. Medication or, in severe circumstances, surgery is used to treat the condition.
Key Facts
- It is not always easy to differentiate between bile reflux and acid indigestion. The symptoms overlap, and the two illnesses may occur simultaneously.
- Peptic ulcers, gall bladder surgeries, and surgery complications like partial or total stomach removal can cause bile reflux.
- Bile Reflux is also called alkaline reflux gastritis.
- Acid reflux is usually easier to manage than bile reflux.
- Chronic bile reflux can damage your stomach and esophageal linings.
Symptoms
Bile reflux and gastric acid reflux often have similar manifestations. The symptoms overlap, and the two conditions may occur simultaneously.
Symptoms of bile reflux include:
- Pain in the upper abdomen, which may be severe.
- Nausea
- Heartburn
- Greenish-yellow vomit
- Regurgitation
- Sore throat
- Indigestion
- Intermittent cough or hoarseness
- Spontaneous weight loss
Diagnosis
Symptoms of bile reflux can manifest in both the stomach and the throat. Reflux into the oesophagus can be diagnosed simply by observing the patient’s symptoms, but stomach reflux will require imaging testing to confirm.
Your healthcare professional may recommend an upper endoscopy examination to observe the internal aspect of your oesophagus, stomach, and upper small intestine (duodenum). In addition to capturing images, the endoscope is equipped with a sample collection tool for analysing tissue for signs of inflammation, tissue damage, and bile.
To determine if bile is refluxing to your oesophagus, it may be necessary to run further tests.
Below is an overview of the tests for bile reflux:
- Under Endoscopy Exam
During this test, you will have a small camera linked to a tube inserted down your neck and into your stomach and intestines. You will be given sedatives and painkillers to help you relax during the assessment. Tissue samples can be collected with the endoscope for further study in the lab.
- HIDA SCAN
Hepatobiliary iminodiacetic acid (HIDA) scans, also known as scintigraphy, are radiographic imaging tests that follow the path of bile as it travels from the liver to the small intestine. You will need to lie within a scanner bed for one to four hours during the examination.
- Bilic Monitoring System
This test detects bile levels in oesophagus reflux with a photo-colorimetric instrument.
- Esophageal Impedance Test
This analysis is an accurate method of distinguishing acid reflux from bile reflux. It can determine the acidity level of the content that has refluxed into your oesophagus.
A tiny tube (catheter) is inserted into your oesophagus via your nose for the test. To ease discomfort, your throat will be numbed and relaxed with anaesthesia.
The catheter remains in place for 24 hours. During this period, it detects any reflux occurrences and the reflux content and notes any following symptoms.
Causes
Events that could trigger bile reflux include:
- Surgery Complications
The most common surgical procedures that lead to bile reflux are gastric bypass surgery and gastrectomy.
- Peptic Ulcers
When you develop a peptic ulcer, it prevents your stomach from emptying properly through the pyloric valve. Having meals sit there for too long raises gastric pressure. This causes the bile to reflux into the food pipe.
- Cholecystectomy
Many patients with bile reflux have previously undergone cholecystectomy (surgical removal of the gallbladder).
Prevention
You can reduce your risks of bile reflux through the following measures:
Quit smoking: Smoking increases stomach acid and dries saliva, harming the oesophagus.
Maintain a healthy weight: Excessive weight can compress your abdomen, causing refluxes of your abdominal contents.
Lift your mattress: Bile reflux symptoms could be avoided by sleeping with a 4 to 6-inch (10 to 15-centimetre) elevation of your upper torso. Instead of extra pillows, try elevating the head of your bed using blocks or a foam wedge.
Relax: Digestion becomes slower when stressed, which could worsen your reflux symptoms. Deep breathing, meditation, or yoga are some good relaxation practices.
Maintain an upright posture after finishing a meal: It’s recommended to wait at least three hours after eating before getting into bed to prevent refluxes.
Cut back on fatty foods: When you eat a lot of fat, your body’s biliary activities become excessive. This may lead to reflux.
Eat and drink right: The lower esophageal sphincter may be loosened by eating certain foods because they cause the stomach to produce too much acid. Coffee, soda, chocolate, citrus, onions, tomatoes, peppers, and mint should be taken in moderation.
Refrain from excessive alcohol consumption: Alcohol irritates the esophagus and relaxes the lower esophageal sphincter.
Typical Treatments
Medications and dietary changes can effectively treat gastroesophageal reflux disorder (GERD). However, managing bile reflux is more complicated. The difficulty in diagnosing bile reflux as a possible root cause of GERD-like symptoms contributes to the limited information on the effective treatments for bile reflux.
According to the Mayo Clinic, the following medications are used to treat bile reflux:
- Ursodeoxycholic acid: This substance changes your stomach bile content.
- Sucralfate: This medication covers and protects your stomach and esophageal linings, making them less susceptible to damage from acid and bile.
- Adsorbents for bile acids: Bile acid sequestrants are commonly prescribed by doctors, although modern research has shown that they are not as effective as alternative treatments. When using them, you may experience serious adverse effects, like stomach swelling.
Surgical Procedures
Sometimes, medications may be ineffective in alleviating severe bile reflux symptoms. Precancerous alterations may also develop in the stomach or oesophagus. In these circumstances, your doctor may suggest you undergo surgery.
You and your doctor should carefully weigh the benefits and risks of any proposed operation.
Surgical procedures for treating bile reflux include:
Diversion surgery: This procedure involves rerouting bile from the stomach to a new drainage link in the lower small intestine.
Anti-reflux operation: In this treatment method, the lower esophageal sphincter is reinforced by wrapping and stitching the portion of the stomach nearest to it. This surgery can help those who suffer from bile and acid reflux by strengthening the valve. However, there is limited research on the success of surgery in treating bile reflux.
Conclusion
Although they have similar symptoms and may occur together, bile reflux is distinct from acid reflux, less common, and more difficult to manage. Healthcare practitioners have a few strategies for treating bile reflux. Surgery may be an option if drugs are ineffective and the symptoms are severe.
MOST COMMON